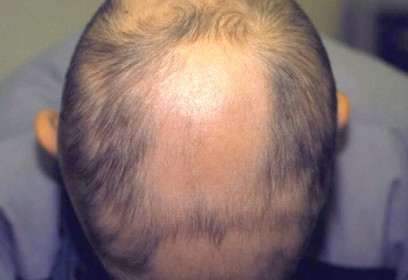
Alopecia areata is a recurrent nonscarring type of hair loss that can affect any hair-bearing area and can manifest in many different patterns. Although it is a benign condition and most patients are asymptomatic, it can cause emotional and psychosocial distress.
Signs and symptoms
Alopecia areata most often is asymptomatic, but some patients (14%) experience a burning sensation or pruritus in the affected area. The condition usually is localized when it first appears, as follows:
- Single patch - 80%
- Two patches - 2.5%
- Multiple patches - 7.7%
No correlation exists between the number of patches at onset and subsequent severity.
Associated conditions may include the following:
- Scalp - 66.8-95%
- Beard - 28% of males
- Eyebrows - 3.8%
- Extremities - 1.3%
Associated conditions may include the following:
- Atopic dermatitis
- Vitiligo
- Thyroid disease
- Collagen-vascular diseases
- Down syndrome
- Psychiatric disorders - Anxiety, personality disorders, depression, and paranoid disorders
- Stressful life events in the 6 months before onset
Alopecia areata can be classified according to its pattern, as follows:
- Reticular - Hair loss is more extensive and the patches coalesce
- Ophiasis - Hair loss is localized to the sides and lower back of the scalp
- Sisaipho (ophiasis spelled backwards) - Hair loss spares the sides and back of the head
- Alopecia totalis - 100% Hair loss on the scalp
- Alopecia universalis - Complete loss of hair on all hair-bearing areas
Nail involvement, predominantly of the fingernails, is found in 6.8-49.4% of patients, most commonly in severe cases. Pitting is the most common; other reported abnormalities have included trachyonychia, Beau lines, onychorrhexis, onychomadesis, koilonychias, leukonychia, and red lunulae.
See Clinical Presentation for more detail.
Diagnosis
Diagnosis usually can be made on clinical grounds. A scalp biopsy seldom is needed, but it can be helpful when the clinical diagnosis is less certain.
See Workup for more detail.
Management
Treatment is not mandatory, because the condition is benign, and spontaneous remissions and recurrences are common. Treatment can be topical or systemic.
Corticosteroids
Intralesional corticosteroid therapy is usually recommended for alopecia areata with less than 50% involvement. Administration is as follows:
- Injections are administered intradermally using a 3-mL syringe and a 30-gauge needle
- Triamcinolone acetonide (Kenalog) is used most commonly; concentrations vary from 2.5-10 mg/mL
- The lowest concentration is used on the face
- A concentration of 5 mg/mL is usually sufficient on the scalp
- Less than 0.1 mL is injected per site, and injections are spread out to cover the affected areas (approximately 1 cm between injection sites)
- Injections are administered every 4-6 weeks
Topical corticosteroid therapy can be useful, especially in children who cannot tolerate injections. It is administered as follows:
- Fluocinolone acetonide cream 0.2% (Synalar HP) twice daily or betamethasone dipropionate cream 0.05% (Diprosone) has been used
- For refractory alopecia totalis or alopecia universalis, 2.5 g of clobetasol propionate under occlusion with a plastic film 6 days/wk for 6 months helped a minority of patients
- Treatment must be continued for a minimum of 3 months before regrowth can be expected, and maintenance therapy often is necessary
Systemic corticosteroids (ie, prednisone) are not an agent of choice for alopecia areata because of the adverse effects associated with both short- and long-term treatment. Some patients may experience initial benefit, but the dose needed to maintain cosmetic growth is usually so high that adverse effects are inevitable, and most patients relapse after discontinuation of therapy.
Immunotherapy
- Topical immunotherapy is defined as the induction and periodic elicitation of an allergic contact dermatitis by topical application of potent contact allergens
- Commonly used agents include squaric acid dibutylester (SADBE) and diphencyprone (DPCP)
Anthralin
- Both short-contact and overnight treatments have been used
- Anthralin concentrations varied from 0.2-1%
Minoxidil
- Minoxidil appears to be effective in the treatment of extensive disease (50-99% hair loss) but is of little benefit in alopecia totalis or alopecia universalis
- The 5% solution appears to be more effective
- No more than 25 drops are applied twice per day regardless of the extent of the affected area
- Initial regrowth can be seen within 12 weeks, but continued application is needed to achieve cosmetically acceptable regrowth
Psoralen plus UV-A
- Both systemic and topical PUVA therapies have been used
- 20-40 treatments usually are sufficient in most cases
- Most patients relapse within a few months (mean, 4-8 months) after treatment is stopped
Other agents
- Topical cyclosporine has shown limited efficacy
- Topical tacrolimus
- Methotrexate, with or without systemic corticosteroids, has shown mixed results
Cosmetic treatment
- Dermatography has been used to camouflage the eyebrows of patients with alopecia areata; on average, 2-3 sessions lasting 1 hour each were required for each patient
- Hairpieces are useful for patients with extensive disease